LGBTQ+ Elder Health Care Guide
Growing older presents challenges for millions of Americans, but members of the LGBTQ+ community are particularly hard-hit. According to the UCLA Williams Institute, LGBTQ+ older adults face many additional barriers to receiving health care. We created this guide to connect the elders of the LGBTQ+ community to the resources and information necessary to help them find the care that they need.

- Written by Christian Simmons
Christian Simmons
Financial Writer
Christian Simmons is a writer for RetireGuide and a member of the Association for Financial Counseling & Planning Education (AFCPE®). He covers Medicare and important retirement topics. Christian is a former winner of a Florida Society of News Editors journalism contest and has written professionally since 2016.
Read More- Edited By
Savannah Pittle
Savannah Pittle
Senior Financial Editor
Savannah Pittle is a professional writer and content editor with over 16 years of professional experience across multiple industries. She has ghostwritten for entrepreneurs and industry leaders and been published in mediums such as The Huffington Post, Southern Living and Interior Appeal Magazine.
Read More- Published: July 26, 2022
- Updated: December 19, 2024
- 11 min read time
- This page features 8 Cited Research Articles
- Edited By
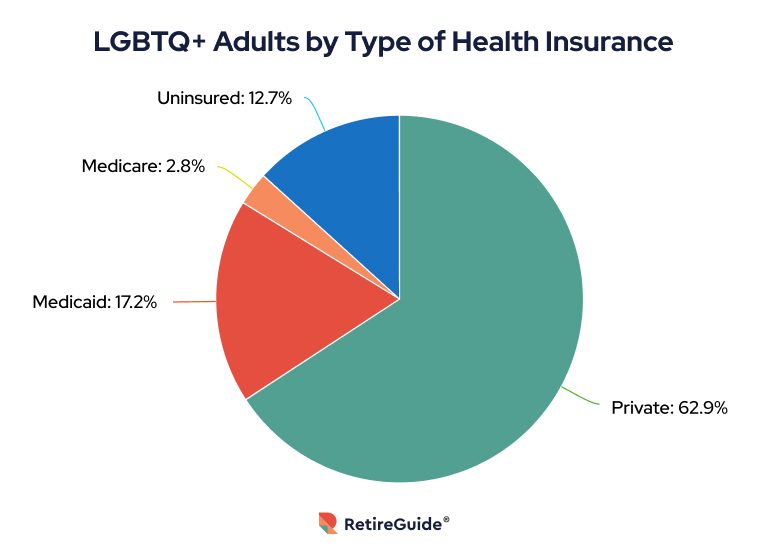
Why Do LGBTQ+ Elders Have Low Rates of Health Insurance?
Several factors contribute to historically lower rates of health insurance among the LGBTQ+ population. One major cause for this trend has been the failure of companies to treat same-sex couples and opposite-sex couples equally in their benefits offerings.
The Kaiser Family Foundation found that the number of firms offering health care coverage to same-sex couples increased from just 43% in 2016 to 74% in 2020. If this upward trend continues, easier access to health care for more members of the LGBTQ+ community will be possible.
Though rates have improved markedly over the last decade, many companies — especially small businesses — still fail to offer health insurance options to same-sex spouses of employees today. While the number of employers offering of same-sex spousal coverage has increased, the benefit remains less common than opposite-sex spousal coverage.
And the damage has been done, especially considering the lack of access to spousal benefits for the decades before same-sex marriage was legalized.
Carey Candrian, PhD, is an associate professor at the University of Colorado School of Medicine who has extensively researched issues relating to health care and LGBTQ+ older adults.
“One out of three older LGBT adults live at or below the poverty level,” Candrian told RetireGuide. “Same-sex marriage wasn’t legalized until 2015. They weren’t married, which means they often were denied spousal benefits and pensions, which really matter as you age and really affect your financial security.”
This lack of access to health care has resulted in more worrying health care trends among the LGBTQ+ community. A Center of American Progress analysis of a 2007 California health survey found that LGBT adults were significantly less likely to seek out the medical care that they need.
And there are further hurdles for members of the community to overcome beyond receiving access to care. Biases and differences in the quality of health care received are realities that many members of the LGBTQ+ community face.
“Health care from the perspective of a bisexual woman has always had a grim outlook. While some health care providers are respectful and open-minded to treatment, that isn’t always the case,” 23-year-old Kirsten Hyman, who has private insurance through the military, told RetireGuide. “There are challenges to finding a provider that will understand you and your values while not imposing their own. I have had many providers turn me away or even discourage me from seeking the answers I need all because my views do not align with theirs.”
Transgender people, in particular, face higher incidences of bias from health care workers. While lesbian, gay and bisexual (LGB) elders might opt not to disclose their sexual orientation or gender identity to their doctors, members of the trans community may not be able to do the same if they are gender nonconforming.
With lower rates of health insurance and more bias faced when attempting to receive care, LGBTQ+ individuals simply don’t seek health care or receive treatment as often as their heterosexual counterparts. In fact, 29% of LGBT adults said they would delay or not seek medical care — compared to just 17% of heterosexual adults — when surveyed.
What Health Care Challenges Do LGBTQ+ Elders Face?
According to the American Psychological Association, over 2.4 million Americans 65 and older identify as part of the LGBT community. And there is a significant health care disparity between the LGBTQ+ community and the rest of the population.
According to Services & Advocacy for Gay, Lesbian, Bisexual & Transgender Elders (SAGE), there are several key areas of the health care system where LGBTQ+ elders experience care disparities.
These include access to health care, treatment for HIV and AIDS, prevalence of mental health conditions and risk for chronic physical conditions. Experiences of discrimination further exacerbate these disparities.
According to Candrian, financial security, a lifetime of discrimination and a significant lack of family support also play a role.
“LGBT older adults are two to three times less likely to be married and they’re three to four times less likely to have kids,” Candrian said. “And they’re also more likely to be estranged from family and even friends. So, they really are aging with a very thin network of support.”
Discrimination
An unfortunate reality for many members of the LGBTQ+ community in the health care system is a difference in treatment by doctors and other health care workers. Discrimination can range from doctors simply not understanding the issues LGBTQ+ adults face to actual denial of service over a patient’s gender identity or sexual orientation.
“Only one or two therapists I’ve ever met actually understood what we go through. Actual medical doctors, they don’t get it,” Casey Jenkins, who identifies as bisexual, told RetireGuide. “I still think it makes my life significantly easier if I just say I’m straight, so doctors don’t think I’m complicated.”
SAGE reports that LGB adults are also more likely to delay getting or not get the prescription drugs that they need and are more likely to receive care in emergency rooms due to fear of discrimination by doctors and facilities providing preventive and nonemergency care.
I still think it makes my life significantly easier if I just say I’m straight, so doctors don’t think I’m complicated.
Facing discrimination during a time in life when health care is critical alters the quality of care received and makes LGBTQ+ elders less likely to go to the doctor when a problem arises — and makes them less likely to stay healthy.
Greater Risk
Another exacerbating factor is that LGBTQ+ elders are at greater risk for numerous serious health conditions, both mental and physical.
For instance, HIV and AIDS heavily affect the LGBTQ+ community. While often portrayed as a serious issue facing young people, 20% of new HIV infections in 2019 were among adults 45 and older, according to the U.S. Centers for Disease Control and Prevention.
LGBTQ+ individuals also disproportionately experience mental health issues. According to the National Alliance on Mental Illness, LGB adults are more than twice as likely to have a mental health condition than heterosexual adults are. Compounding the issue is a lack of access to mental health services for LGBTQ+ adults because of both discrimination and lack of health insurance.
There are many other conditions that LGBTQ+ members may be at higher risk of as well, ranging from diabetes to cancer.
Medicare Bill Rejections
Medicare bill rejections are another critical area contributing to disparities in care for LGBTQ+ individuals.
Because Medicare codes some services specifically to gender — meaning that computer systems automatically link them to “male” or “female” beneficiaries — these rejections are an especially serious issue for transgender people.
Consider a transgender woman age 50 or over who has the medical necessity to receive an annual prostate exam screening. If her identification has been updated, Medicare’s system may not understand why a woman needs a prostate exam and automatically reject the claim.
Having outdated and incorrect gender identity information on government documents like driver’s licenses or Medicare cards can also lead to Medicare bill rejections for many transgender individuals.
Does Medicare Cover Gender-Affirming Services?
Medicare will cover some gender-affirming services, but coverage depends on both the specific service and the individual situation. Coverage decisions are made on the following treatments and procedures on a case-by-case basis.
Surgery
Original Medicare will cover and pay for gender-affirming surgery in some cases.
Medicare’s defining principle for determining coverage in any scenario is whether the service is considered medically necessary. For gender-affirming surgery, medical necessity is currently determined on a case-by-case basis by local administrators.
Gender reassignment surgery is covered when the operation is deemed “reasonable and necessary” for the beneficiary after evaluating the person’s unique circumstances.
Likewise, each individual Medicare Advantage plan determines whether surgery is reasonable and medically necessary for a beneficiary.
Medicare, however, is unlikely to cover procedures like facial feminization or facial masculinization surgeries because they are considered cosmetic.
Hormone Therapy
Hormone therapy may be covered as part of a gender-affirming transition when a doctor deems the therapy medically necessary.
But again, individual circumstances may vary since Medicare has no national coverage determination for this topic and leaves it up to case-by-case decisions.
| Procedure or Service | When Medicare Covers It |
|---|---|
| Gender-Affirming Surgery | On a case-by-case basis and when it is deemed medically necessary. Hormone therapy may be required first to prove medical necessity. |
| Hormone Therapy | On a case-by-case basis and when it is deemed medically necessary. |
| Additional Procedures Like Facial Masculinization/Feminization | Unlikely to be covered. |
If Medicare denies your claim and your doctor believes the surgery or procedure is reasonable and medically necessary, you can appeal Medicare’s decision.
What Protections Are in Place for LGBTQ+ Elder Patients?
According to Health Affairs, there are specific protections in place through the Affordable Care Act for LGBTQ+ elder patients.
These rules prohibit discrimination against an individual in the LGBT community. But while these rules do exist, discrimination does still happen and the Act’s specific rules continue to be debated on the political stage.
According to Candrian, there can be a disconnect between the laws and regulations in place and what actually occurs within the health care system.
“Discrimination polices are great, but not if they don’t trickle down and people actually aren’t aware of how to enforce them,” she said. “Organizational-wide education is critical to even know that these issues exist and they have really concrete effects.”
What To Do If You Encounter Health Care Discrimination
Unfortunately, there are few direct and impactful options available to LGBTQ+ elders to rectify a situation where they’ve faced discrimination when attempting to receive health care.
According to the Human Rights Campaign, the majority of hospitals have grievance processes where patients can report the discrimination they have faced. You may also file a complaint through your state’s health department.
But response or action could be weeks — or months — away.
“It’s already so hard to get in to see a provider and so expensive to see a provider, but then if you do speak up, if the provider gets upset they can literally ask you to leave,” Candrian said. “It’s up to [the patient] to really have the courage to speak up.”
Why Is It Important To Have an Inclusive Doctor?
LGBTQ+-identifying Americans have to deal with many issues when seeking health care that heterosexual adults don’t have to think twice about — like whether it is safe for them to be honest about intimate and personal details.
Seeing an inclusive doctor allows LGBTQ+ elders to feel comfortable sharing personal information that is important to their health care needs, including their sexual orientation and gender identity.
Having an inclusive doctor can not only improve the trust and support that LGBTQ+ elders feel from doctor’s visits, but also actually improve the quality of care.
A doctor who actually understands the needs of elders of this community as well as the disparities and additional issues that they face can make a big difference.
How To Find an Inclusive Health Care Professional
It can be difficult to find an inclusive doctor depending on where you are in the country, with some regions having better resources than others.
The provider directory from Health Professionals Advancing LGBTQ Equality can help you find trustworthy, inclusive doctors near you.
When searching for doctors in your area, some may clarify that they are LGBTQ+-friendly. But it’s also worth asking other LGBTQ+ elders in your area about where they are receiving their health care and if they have had any issues with their current providers.
Health Care Resources for LGBTQ+ Elders
There are many resources available to LGBTQ+ elders, ranging from mental health services and support groups to organizations that can direct you towards helpful information and inclusive health care. There may be local resources available near where you live as well.
Mental Health Resources
The 988 Suicide & Crisis Lifeline is available 24 hours a day at 988 and someone equipped to help is waiting to answer at all times.
For LGBTQ+-specific services, the National Alliance on Mental Illness offers tips and steps on how members of the community can find the right mental health professionals for their unique set of circumstances.
The American Foundation for Suicide Prevention includes links to several lifelines and chats, including those specifically for elders and members of the trans community.
The SAGE LGBT Elder Hotline can be reached here.
The Human Rights Campaign can connect you with many additional LGBTQ+-focused mental health resources.
Support Groups
There may be support groups and local resources available where you live.
The National Resource Center on LGBTQ+ Aging offers a very extensive list of helplines, groups, centers and resources for LGBTQ+ seniors that span across the country.
There are also links to and information about support groups and networks available from Iona.
You can search the internet for support groups within your local area. Support groups exist across the country and you have a good chance of finding one nearby.
Organizations
SAGE is a national advocacy organization specifically for LGBTQ+ elders. Information ranging from resources and hotlines to information and education is available on their website.
The National Council on Aging is a general organization for all seniors that offers LGBT-specific resources and information on health care services.
There may be local and city-specific organizations available near you as well.
8 Cited Research Articles
- Kaiser Family Foundation. (2020, November 30). Access to Employer-Sponsored Health Coverage for Same-Sex Spouses: 2020 Update. Retrieved from https://www.kff.org/private-insurance/issue-brief/access-to-employer-sponsored-health-coverage-for-same-sex-spouses-2020-update/
- Association of Health Care Journalists. (2018, July 18). National study finds LGBT seniors face tougher old age. Retrieved from https://healthjournalism.org/blog/2018/07/national-study-finds-lgbt-seniors-face-tougher-old-age/
- SAGE. (2018, May). Transgender Older Adults & Medicare Fraud Prevention. Retrieved from https://www.sageusa.org/wp-content/uploads/2018/05/sageusatransgender-older-adults-tipsheet-medicare-fraud-prevention.pdf
- Health Affairs. (2016, June 6). LGBT Protections in Affordable Care Act Section 1557. Retrieved from https://www.healthaffairs.org/do/10.1377/forefront.20160606.055155
- American Psychological Association. (2013). Lesbian, Gay, Bisexual, and Transgender Aging. Retrieved from https://www.apa.org/pi/lgbt/resources/aging
- SAGE. (2010, September). LGBT Older Adults and Health Disparities. Retrieved from https://www.sageusa.org/wp-content/uploads/2018/06/2010-lgbt-older-adults-and-health-disparities.pdf
- Human Rights Campaign. (n.d.). What To Do If You Experience Discrimination. Retrieved from https://www.hrc.org/resources/what-to-do-if-you-experience-discrimination
- National Alliance on Mental Illness. (n.d.). LGBTQI. Retrieved from https://www.nami.org/Your-Journey/Identity-and-Cultural-Dimensions/LGBTQI
Calling this number connects you to one of our trusted partners.
If you're interested in help navigating your options, a representative will provide you with a free, no-obligation consultation.
Our partners are committed to excellent customer service. They can match you with a qualified professional for your unique objectives.
We/Our Partners do not offer every plan available in your area. Any information provided is limited to those plans offered in your area. Please contact Medicare.gov or 1-800-MEDICARE to get information on all of your options.
888-694-0290Your web browser is no longer supported by Microsoft. Update your browser for more security, speed and compatibility.
If you need help pricing and building your medicare plan, call us at 844-572-0696

