Medicare History
Medicare was signed into law July 30, 1965, in a bipartisan effort to provide health care coverage for millions of older Americans. Over its 55-year history, the program has grown to include people with permanent disabilities. It’s also added drug coverage, private insurance options and free preventative services.
- Written by Rachel Christian
Rachel Christian
Financial Writer and Certified Educator in Personal Finance
Rachel Christian is a writer and researcher for RetireGuide. She covers annuities, Medicare, life insurance and other important retirement topics. Rachel is a member of the Association for Financial Counseling & Planning Education.
Read More- Edited By
Lee Williams
Lee Williams
Senior Financial Editor
Lee Williams is a professional writer, editor and content strategist with 10 years of professional experience working for global and nationally recognized brands. He has contributed to Forbes, The Huffington Post, SUCCESS Magazine, AskMen.com, Electric Literature and The Wall Street Journal. His career also includes ghostwriting for Fortune 500 CEOs and published authors.
Read More- Reviewed By
Joe Benish
Joe Benish
Licensed Agent at Insuractive
As a licensed insurance agent specializing in providing seniors with Medicare-related products, Joe Benish knows how daunting it can be to learn about Medicare and all of the options available. That’s why he spends his time getting to know his clients and helping them select the right plans for them from the more than 15 insurance companies he represents.
Read More- Published: December 1, 2020
- Updated: December 19, 2024
- 12 min read time
- This page features 38 Cited Research Articles
- Edited By
History of Medicare
Medicare, established in 1965, provides health insurance to Americans aged 65 and older and to younger people with disabilities.
The federal program has evolved significantly over time to give more Americans access to the quality and affordable health care they need.
From its inclusion of people with long-term disabilities in 1972 to the creation of Medicare Part D drug coverage in the early 2000s, Medicare continues to adapt to a changing health care landscape.
More than 62 million people are now enrolled in Medicare, and it remains one of the country’s most popular federal programs.
-
1945
Harry Truman becomes the first president to propose national health insurance legislation.
-
1960
The Medical Assistance to the Aged, also known as the Kerr-Mills Act, is signed into law. It provides limited health care assistance to the elderly and features elements of the future Medicare program.
-
July 30, 1965
President Lyndon B. Johnson enacts Medicare by signing the Social Security Amendments of 1965 (H.R. 6675) into law in Independence, Missouri.
-
July 1, 1966
Medicare goes into effect. More than 19 million Americans aged 65 and older enroll.
-
1972
Medicare eligibility is extended to people under age 65 with long-term disabilities and to individuals with end-stage renal disease.
-
August 5, 1997
President Bill Clinton signs the Balanced Budget Act of 1997. It creates the Medicare+Choice program, a predecessor to modern Medicare Advantage plans.
-
December 8, 2003
President George W. Bush signs the Medicare Prescription Drug, Improvement, and Modernization Act, or MMA. It is considered the biggest reform since Medicare’s inception.
Under the MMA, private health plans approved by Medicare are renamed Medicare Advantage plans.
-
January 1, 2006
Medicare Part D goes into effect.
-
March 23, 2010
President Barack Obama signs the Affordable Care Act. It expands Medicare coverage to include several free preventative services and helps close the Part D donut hole.
Early Attempts at National Health Insurance
Discussions of a federal health care system began decades before Medicare’s inception.
In the 1930s, President Franklin Delano Roosevelt decided not to add health care to his Social Security proposal because he feared it would be too controversial and might hinder the passage of other legislation.
President Harry Truman picked up the fight during his administration and took things a step further with a plan to protect a greater number of Americans.
Medicare for All may seem like a new idea, but Truman proposed national health insurance for every American in 1945, and again in 1949.
Millions of our citizens do not now have a full measure of opportunity to achieve and enjoy good health. Millions do not now have protection or security against the economic effects of sickness. The time has arrived for action to help them attain that opportunity and that protection.
Truman insisted that he was not in favor of “socialized medicine” noting that “the American people want no such system.”
But like modern efforts to expand the federal government’s role in health care, Truman’s attempts were met with staunch opposition.
The American Medical Association and other special interest groups launched expensive lobbying campaigns to kill the bill.
The efforts were successful. By 1950, Truman’s latest proposal was dead.
The idea of a smaller, more targeted program for people aged 65 and older began to emerge in the late 1950s.
Several Democrats introduced legislation that focused on giving elderly Americans health care benefits funded with payroll taxes and overseen by the Social Security Administration.
The media dubbed these proposals Medicare.
The idea gained momentum as organized labor unions backed the proposal. By 1960, presidential candidate John F. Kennedy publicly endorsed the idea.
That same year, the Kerr-Mills Act was signed into law. It created a new means-tested program known as Medical Assistance for the Aged. It also provided federal grants to states that covered health care costs for low-income seniors.
At the time, it was considered a good compromise.
However, three years later, less than 1 percent of older Americans were covered, only 32 states had implemented the legislation and large coverage discrepancies existed across the country.
Kennedy wanted Congress to take bolder action.
“The fact of the matter is that what we are now talking about doing, most of the countries of Europe did years ago,” Kennedy said at a 1962 New York rally. “We are behind every country, pretty nearly, in Europe, in this matter of medical care for our citizens.”
Kennedy never saw the vision realized, but his successor, Lyndon B. Johnson, made Medicare a reality just three years later.
Signing Medicare into Law
When Johnson was elected in 1964, he was determined to pass sweeping social reforms on level with the New Deal.
Health insurance for seniors was at the top of his list.
“Our older people are likely to be hospitalized three times as often as younger people, but their income is less than half of that for people under 65,” Johnson said during a White House briefing January 1964.
On July 30, 1965, Johnson signed Medicare into law at a public ceremony in Independence, Missouri. Former President Truman was by his side.
After signing the Social Security Amendments of 1965, Johnson turned to Truman, now 81, and proclaimed him “the real daddy of Medicare.”
Truman also became the first person to enroll in the program.
Once the festivities ended, the real work began.
Wilbur Cohen, undersecretary of Health, Education and Welfare, said the task of enrolling millions of Americans into the new system in less than a year was like planning the invasion of Normandy.
“We did a better job of preparation than we did for almost any other program,” Cohen said.
When Medicare services launched July 1, 1966, more than 19 million Americans aged 65 and older enrolled.
We think this program is just. We think this program is necessary. We think this program makes sense. And we think this program is going to be the law of the land.
Prior to its creation, only about half of people over age 65 had health insurance.
Medicare rapidly shrank the number of elderly citizens lacking access to hospitals and doctors in the United States.
It also played a unique role in the civil rights movement.
The year prior to Medicare’s passage, the Civil Rights Act of 1964 had barred federal funding from institutions that discriminated based on race.
Because Medicare was the first national health care program, Southern hospitals were forced to integrate or risk losing funding. Field inspectors visited hospitals to ensure compliance.
It proved to be a powerful motivator.
It’s estimated that more than 1,000 hospitals in the South integrated in less than four months following Medicare’s passage.
The original 1965 amendments to the Social Security program consisted of three parts — hospital insurance financed by payroll taxes, doctor coverage paid for by individual premiums and state grants to be used for the nation’s poorest residents. This last part became the modern Medicaid program.
Today, Medicare Part A pays for a portion of hospital stays, some home health care, skilled nursing facilities and hospice. Most people don’t pay a monthly fee, or premium, for Part A because it’s funded by payroll taxes.
Medicare Part B covers doctor visits and other services. Everyone is required to pay a premium for Part B or, in the case of qualifying low-income individuals, have premiums paid on their behalf by state agencies.
Medicare Continues to Evolve
In 1972, Medicare eligibility was extended to people under age 65 with long-term disabilities and individuals with end-stage renal disease.
The idea was to provide a fallback for people who carry substantial medical expenses but who are unable to get insurance through their employers.
By 2020, 8.5 million younger people received Medicare coverage for the disabled, or about 13.6 percent of all beneficiaries.
History of Medicare Advantage and Private Insurance
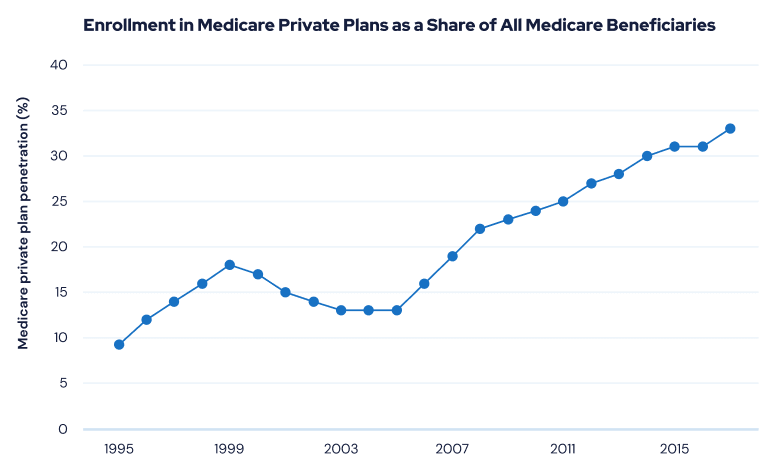
Private Medicare health insurance plans have existed in some form since the 1970s. At that time, only health maintenance organizations, or HMOs, were available.
The modern Medicare Advantage program was first established as Medicare+Choice, or Part C, by the Balanced Budget Act of 1997.
The law overhauled the previous payment formula and updated the risk-adjustment model. In an attempt to reduce spending, it also lowered payment rates to private plans.
The law created several new plan options, including preferred provider organizations, provider-sponsored organizations, private fee-for-service plans and high-deductible plans with medical savings accounts.
- Reduce government cost
- Expand choices for consumers
- Enhance health care quality
However, the program was considered unsuccessful.
The reduced payment rate caused a wave of plans to exit the program.
In 2000, of the existing participating plans, 99 withdrew, affecting 327,000 people. In 2001, withdrawals and service area reductions affected about 934,000 enrollees.
Insurers cut extra benefits and increased cost-sharing among members as the free market adjusted to the change.
Enrollment in Medicare+Choice plans dropped nearly 30 percent between 1999 and 2003. Meanwhile, the average premium across all private plans skyrocketed 260 percent from 1999 to 2001.
In 2003, Medicare+Choice was modified under a new law and renamed Medicare Advantage.
The new law significantly raised payments to private plans to counter the effects of the Balanced Budget Act. Medicare began offering rates that were at least as high as Original Medicare spending per enrollee.
A new bidding process was also established where every plan submits a bid representing its estimated cost of providing basic Medicare benefits to enrollees for the coming year.
The private Medicare insurance market boomed in response, and enrollment continues to grow.
From 2010 to 2017, Medicare Advantage enrollment increased more than 70 percent.
By 2023, nearly half of all Medicare beneficiaries — or 30 million people — were enrolled in Medicare Advantage plans, according to the Kaiser Family Foundation.
Today, Medicare Advantage plans are required to provide at least the same benefits as Original Medicare. They often bundle coverage for other services — including prescription drugs, dental and vision — into a single plan.
Medicare Part D Launches
In 2003, President George W. Bush signed the Medicare Prescription Drug, Improvement, and Modernization Act, or MMA.
Many experts consider it the largest overhaul to Medicare since the program’s inception.
The MMA established Medicare Part D, which provides millions of seniors with prescription drug coverage through a complex system of subsidies to private insurance companies. Beneficiaries also pay into the program with monthly premiums.
For beneficiaries with limited resources, the Social Security Administration and CMS work together to provide special low-income subsidies.
The Part D program was phased in and went into full effect Jan. 1, 2006.
One key provision of the law has remained controversial. The legislation did not allow the federal government to negotiate drug prices. Instead, it explicitly states that only insurance companies administering Medicare prescription drug programs have the legal right to negotiate drug prices directly with manufacturers.
As drug prices soared, the provision stood out as a potential barrier to lower consumer costs because the government was unable to leverage its purchasing power with pharmaceutical companies.
Repealing the provision has broad public support, with a 2015 Kaiser Family Foundation poll showing 88 percent of Americans holding a favorable view of the idea.
Over the years, members of Congress have proposed multiple bills to revise this provision — with no success.
Affordable Care Act Grants Free Preventative Services to Medicare Users
President Barack Obama signed the Affordable Care Act into law March 23, 2010.
The sweeping health care reform added many preventative services to Medicare coverage — including exams, shots, lab tests and screenings.
These services are offered to beneficiaries for free with no deductible, copayment or coinsurance.
- An annual wellness visit
- Cancer screening tests, such as mammograms and colonoscopies
- Diabetes screening and self-management training
- Tobacco cessation counseling
- High cholesterol and high blood pressure screenings
- A Welcome to Medicare visit
- Flu and pneumonia shots
- STD and HIV testing
Eliminating cost barriers for preventative services has three primary goals: Improve people’s short- and long-term health outcomes, increase workplace productivity and reduce the nation’s health care costs.
The ACA also took measures to close the prescription drug coverage gap, also known as the Medicare Part D donut hole.
Previously, when seniors exceeded a certain amount in their annual prescription drug costs, they were forced to pay all the costs of their prescriptions in this gap.
The ACA phased out the coverage gap by requiring Part D plans to pay a gradually larger share of total drug costs. It also forced drug manufacturers to give discounts on the drugs in the gap.
Inflation Reduction Act Expected To Lower Drug Costs for Medicare Beneficiaries
On August 16, 2022, President Biden signed into law the Inflation Reduction Act of 2022, a far-reaching piece of legislation that addresses climate change, taxes and healthcare. Included in the bill are provisions designed to lower prescription drug costs for people with Medicare.
There are two main policies featured in the Inflation Reduction Act that influence prescription drug prices. The first requires the federal government to negotiate with drug companies to get lower prices on some high-cost drugs covered under Medicare Part D and Part B. The list of drugs that can be negotiated starts small with just 10 Part D medications in 2026, and will expand in subsequent years to include more Part D and Part B drugs.
The second provision is designed to discourage drug companies from rapidly raising their prices. Under the Inflation Reduction Act, pharmaceutical manufacturers must pay rebates to Medicare if they increase prices faster than inflation for drugs used by Medicare beneficiaries. This inflation rebate requirement will take effect in 2023 and will use 2021 prices as a benchmark for determining price changes relative to inflation.
In addition to these provisions, the Inflation Reduction Act also includes policies capping out-of-pocket spending for Medicare Part D beneficiaries, limiting annual increases in Part D premiums for 2024 to 2030, and lowering cost sharing for insulin to $35 per month for people with Medicare.
38 Cited Research Articles
- Centers for U.S. Medicare & Medicaid Services. (2023, October 12). 2024 Medicare Parts A & B Premiums and Deductibles. Retrieved from https://www.cms.gov/newsroom/fact-sheets/2024-medicare-parts-b-premiums-and-deductibles
- U.S. Centers for Medicare & Medicaid Services. (2022, September 27). 2023 Medicare Parts A and B Premiums and Deductibles 2023 Medicare Part D Income-Related Monthly Adjustment Amounts. Retrieved from https://www.cms.gov/newsroom/fact-sheets/2023-medicare-parts-b-premiums-and-deductibles-2023-medicare-part-d-income-related-monthly
- Freed, M., et al. (2022, August 25). Medicare Advantage in 2022: Enrollment Update and Key Trends. Retrieved from https://www.kff.org/medicare/issue-brief/medicare-advantage-in-2022-enrollment-update-and-key-trends/
- Centers for Medicare & Medicaid Services. (2022, August 20). CMS Fast Facts. Retrieved from https://data.cms.gov/fact-sheet/cms-fast-facts
- Cubanski, J., et al. (2022, August 18). How Will the Prescription Drug Provisions in the Inflation Reduction Act Affect Medicare Beneficiaries? Retrieved from https://www.kff.org/medicare/issue-brief/how-will-the-prescription-drug-provisions-in-the-inflation-reduction-act-affect-medicare-beneficiaries/
- Gritter, M. (2019, August 20). The Kerr–Mills Act and the Puzzles of Health‐Care Reform. Retrieved from https://onlinelibrary.wiley.com/doi/abs/10.1111/ssqu.12714
- Abrams, A. (2019, May 30). The Surprising Origins of 'Medicare for All.’ Retrieved from https://time.com/5586744/medicare-for-all-history/
- Cubanski, J., Neuman, T. and Damico, A. (2018, August 21). Closing the Medicare Part D Coverage Gap: Trends, Recent Changes, and What’s Ahead. Retrieved from https://www.kff.org/medicare/issue-brief/closing-the-medicare-part-d-coverage-gap-trends-recent-changes-and-whats-ahead/
- Patel, Y. M. and Guterman, S. (2017, December 8). The Evolution of Private Plans in Medicare. Retrieved from https://www.commonwealthfund.org/publications/issue-briefs/2017/dec/evolution-private-plans-medicare
- Jacobson, G. et al. (2017, June 6). Medicare Advantage 2017 Spotlight: Enrollment Market Update. Retrieved from https://www.kff.org/medicare/issue-brief/medicare-advantage-2017-spotlight-enrollment-market-update/
- Cubanski, J. et al. (2016, December 13). What Are the Implications of Repealing the Affordable Care Act for Medicare Spending and Beneficiaries? Retrieved from https://www.kff.org/health-reform/issue-brief/what-are-the-implications-of-repealing-the-affordable-care-act-for-medicare-spending-and-beneficiaries/
- Theodore, T., Abbe, L. R. and Gluck, D. (2016, September 19). The Politics of Medicare and Drug-Price Negotiation Updated. Retrieved from https://www.healthaffairs.org/do/10.1377/forefront.20160919.056632/full/
- Biles, B., Casillas, G. and Guterman, C. (2015, August 25). Competition Among Medicare’s Private Health Plans: Does It Really Exist? Retrieved from https://www.commonwealthfund.org/publications/issue-briefs/2015/aug/competition-among-medicares-private-health-plans-does-it-really?redirect_source=/publications/issue-briefs/2015/aug/competition-medicare-private-plans-does-it-exist
- Cubanski, J., Neuman, T. and Damico, A. (2016, August 12). Medicare's Role for People Under Age 65 with Disabilities. Retrieved from https://www.kff.org/medicare/issue-brief/medicares-role-for-people-under-age-65-with-disabilities/
- NPR. (2015, July 30). 50 Years Ago, Medicare Helped To Desegregate Hospitals. Retrieved from https://www.npr.org/2015/07/30/427648586/50-years-ago-medicare-helped-to-desegregate-hospitals
- Sternberg, S. (2015, July 29). Desegregation: The Hidden Legacy of Medicare. Retrieved from https://www.usnews.com/news/articles/2015/07/30/desegregation-the-hidden-legacy-of-medicare
- Norton, M., DiJulio, B. and Brodie, M. (2015, July 17). Medicare And Medicaid At 50. Retrieved from https://www.kff.org/medicaid/poll-finding/medicare-and-medicaid-at-50/
- Centers for Medicare & Medicaid Services. (2015, July). Medicare and Medicaid Milestones. Retrieved from https://www.cms.gov/About-CMS/Agency-Information/History/Downloads/Medicare-and-Medicaid-Milestones-1937-2015.pdf
- Davis, K., Guterman, S. and Bandeali, F. (2015, June 9). The Affordable Care Act and Medicare. Retrieved from https://www.commonwealthfund.org/publications/fund-reports/2015/jun/affordable-care-act-and-medicare
- Kaiser Family Foundation. (2015, April 21). Medicare and Medicaid at 50. Retrieved from https://www.youtube.com/watch?v=f9NUCvrrRz4
- Kaiser Family Foundation. (2015, March 24). Medicare: 50 Years and Counting Timeline. Retrieved from https://www.kff.org/medicare/timeline/medicare-timeline/
- Markel, H. (2015, March). Give ’Em Health, Harry. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4364422/
- Zelizer, J. (2015, February 15). How Medicare Was Made. Retrieved from https://www.newyorker.com/news/news-desk/medicare-made
- Markel, H. (2014, November 19). 69 years ago, a president pitches his idea for national health care. Retrieved from https://www.pbs.org/newshour/health/november-19-1945-harry-truman-calls-national-health-insurance-program
- Stanton, M. (2013, July). Medicare Turns 48. Retrieved from https://www.aarp.org/health/medicare-insurance/info-07-2013/medicare-anniversary-july-30-1965.html
- Mcguire, T. G., Newhouse, J. P. and Sinaiko, A. D. (2011, June). An Economic History of Medicare Part C. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3117270/
- Centers for Medicare & Medicaid Services. (2010, July 14). Background: The Affordable Care Act’s New Rules on Preventive Care. Retrieved from https://www.cms.gov/CCIIO/Resources/Fact-Sheets-and-FAQs/preventive-care-background
- The Commonwealth Fund. (2002, February 14). Medicare Plus Choice Enrollees Face Rising Out-Of-Pocket Costs; Those In Poor Health Hardest Hit. Retrieved from https://www.commonwealthfund.org/press-release/2002/medicare-plus-choice-enrollees-face-rising-out-pocket-costs-those-poor-health
- Gold, M. (2001, August). Medicare+Choice: An Interim Report Card. Retrieved from https://www.healthaffairs.org/doi/full/10.1377/hlthaff.20.4.120
- The American Presidency Project. (1964, January 15). Lyndon B. Johnson, Remarks to Leaders of Organizations Concerned With the Problems of Senior Citizens. Retrieved from https://www.presidency.ucsb.edu/documents/remarks-leaders-organizations-concerned-with-the-problems-senior-citizens
- The American Presidency Project. (1962, May 20). John F. Kennedy, Address at a New York Rally in Support of the President's Program of Medical Care for the Aged. Retrieved from https://www.presidency.ucsb.edu/documents/address-new-york-rally-support-the-presidents-program-medical-care-for-the-aged
- Centers for Medicare & Medicaid Services. (n.d.). CMS’ program history. Retrieved from https://www.cms.gov/About-CMS/Agency-Information/History
- Centers for Medicare & Medicaid Services. (n.d.). Tracing the History of CMS Programs: From President Theodore Roosevelt to President George W. Bush. Retrieved from https://www.cms.gov/About-CMS/Agency-Information/History/Downloads/BushSignMMA2003.pdf
- Medicare.gov. (n.d.). Your Guide to Medicare Preventive Services. Retrieved from https://web.archive.org/web/20211116192958/https://www.medicare.gov/sites/default/files/2021-08/10110-Your-Guide-to-Medicare-Preventive-Services.pdf
- National Council on Aging. (n.d.). Medicare Low Income Subsidy: Get Extra Help Eligibility and Coverage Chart. Retrieved from https://www.ncoa.org/article/part-d-low-income-subsidy-extra-help-eligibility-and-coverage-chart
- Social Security Administration. (n.d.). History of SSA During the Johnson Administration 1963-1968. Retrieved from https://www.ssa.gov/history/ssa/lbjmedicare1.html
- Social Security Administration. (n.d.). Medicare Program Description and Legislative History. Retrieved from https://www.ssa.gov/policy/docs/statcomps/supplement/2011/medicare.html
- United States Senate. (n.d.). Medicare Signed into Law. Retrieved from https://www.senate.gov/artandhistory/history/minute/Medicare_Signed_Into_Law.htm
Calling this number connects you to one of our trusted partners.
If you're interested in help navigating your options, a representative will provide you with a free, no-obligation consultation.
Our partners are committed to excellent customer service. They can match you with a qualified professional for your unique objectives.
We/Our Partners do not offer every plan available in your area. Any information provided is limited to those plans offered in your area. Please contact Medicare.gov or 1-800-MEDICARE to get information on all of your options.
888-694-0290Your web browser is no longer supported by Microsoft. Update your browser for more security, speed and compatibility.
If you need help pricing and building your medicare plan, call us at 844-572-0696


